- What is Duodenal Switch Surgery?
- How Does Duodenal Switch Surgery Work?
- Duodenal Switch Benefits
- Duodenal Switch Surgery Procedure
- Duodenal Switch Pros and Cons
- Duodenal Switch Surgery and Weight Loss
- Duodenal Switch Surgery Recovery
- Duodenal Switch Candidates
- Duodenal Switch vs. Gastric Sleeve
- Duodenal Switch Diet
- Duodenal Switch Cost
- Duodenal Switch Side Effects
- Open vs. Laparoscopic Surgery
- Bariatric Surgery Options
- Duodenal Switch FAQs
What is Duodenal Switch Surgery?
How Duodenal Switch Weight Loss Surgery Works
The duodenal switch procedure — also known as biliopancreatic diversion with duodenal switch — is a type of weight loss surgery with two components. The first aims to restrict the amount of food that the patient can take in by removing a significant portion of the stomach. The second component aims to prevent full absorption of calories and fat by rerouting and bypassing a significant portion of the small intestine.
Thanks to the combination of food intake restriction and the prevention of calorie absorption, patients undergoing duodenal switch weight loss surgery experience greater weight loss than gastric bypass patients.
What Conditions Can Duodenal Switch Improve?
While there are many weight loss options that can help you take control of your health, duodenal switch surgery in particular offers significant benefits for severely obese patients affected by life-threatening medical conditions. In general, the procedure is only considered when losing weight from dieting and exercise proves unsuccessful. On top of reducing the risks of high blood pressure, sleep apnea, high cholesterol, stroke, and heart disease, the duodenal switch procedure can improve various weight-related conditions like:
- Type 2 diabetes
- Heart disease
- Lung disease
- Sleep apnea
- High blood pressure
- High cholesterol
- Non-alcoholic fatty liver disease
Duodenal switch can also be an excellent means of revision bariatric surgery for men and women who did not lose enough weight from gastric sleeve surgery, or who have gained substantial weight after their initial procedure. Everyone has a different procedure that works for their medical history and health goals, which is why our DFW practice provides a diverse range of potential solutions. Dr. Bagshahi and our team can carefully assess your concerns and recommend the most effective weight loss options for your unique needs.
The Duodenal Switch Surgery Procedure
The duodenal switch procedure typically takes around four hours. The procedure is performed either laparoscopically or as open surgery, depending on the patient.
First, approximately 70% of the stomach is removed. The remaining stomach becomes cylindrical, linking the esophagus to the duodenum, or the top portion of the small intestine.
In the next step the duodenum is divided into two parts, with one part of the small intestine remaining attached to the stomach. A portion of the small intestine is cut, and the distal small intestine (the part closest to the colon) is attached directly to the duodenum.
By doing so, the patient’s food intake will flow directly from the stomach into the colon, bypassing three-quarters of the small intestine resulting in limited caloric absorption.
Advantages and Disadvantages of Duodenal Switch Surgery
Advantages
- Results in greater weight loss than RYGB, LSG, or AGB
- Allows patients to eventually eat near “normal” meals
- Reduces the absorption of fat by 70 percent or more
- Causes favorable changes in gut hormones to reduce appetite and improve satiety
- Is the most effective against diabetes compared to RYGB, LSG, and AGB
Disadvantages
- Has higher complication rates and risk for mortality than the AGB, LSG, and RYGB
- Requires a longer hospital stay than the Adjustable Gastric Band or Laparoscopic Sleeve Gastrectomy
- Has a greater potential to cause protein deficiencies and long-term deficiencies in a number of vitamin and minerals, i.e. iron, calcium, zinc, fat-soluble vitamins such as vitamin D
- Compliance with follow-up visits and care and strict adherence to dietary and vitamin supplementation guidelines are critical to avoiding serious complications from protein and certain vitamin deficiencies
How the Duodenal Switch procedure helps weight loss
Because such a significant portion of the small intestine is bypassed, food intake is not mixed with pancreatic enzymes and bile until it is close to the colon. This delayed mixing results in a reduced absorption of calories and fat.
Similar to other bariatric surgeries, the BPD/DS initially helps to reduce the amount of food that is consumed; however, over time this effect lessens and patients are able to eventually consume near “normal” amounts of food. Unlike the Gastric Sleeve and LAP-BAND®, there is a significant amount of small bowel that is bypassed by the food stream.
Additionally, the food does not mix with the bile and pancreatic enzymes until very far down the small intestine. This results in a significant decrease in the absorption of calories and nutrients (particularly protein and fat) as well as nutrients and vitamins dependent on fat for absorption (fat soluble vitamins and nutrients).
Lastly, the BPD/DS, similar to the Gastric Bypass and Sleeve Gastrectomy, affects gut hormones in a manner that impacts hunger and satiety as well as blood sugar control. The BPD/DS is considered to be the most effective surgery for the treatment of diabetes among those that are described here.
Recovery from Duodenal Switch Weight Loss Surgery
Duodenal switch patients typically remain in the hospital for a few days after surgery. The hospital monitors patients to ensure that there are no complications from the surgery, such as staple leaks, and to confirm that the rerouted digestive system is functioning correctly.
Most duodenal switch patients have a follow-up appointment with their surgeon a month later, with additional follow-up visits quarterly for the first year and twice a year thereafter. At first, duodenal switch patients are only able to consume a reduced portion of food; over time, the amount of food patients are able to take in will increase, while the resulting lower caloric absorption will remain. In addition, patients are required to follow careful dietary guidelines with a vitamin supplement regime.
Our Fellowship-trained bariatric surgeon—Dr. Hossein Bagshahi—is pleased to offer patients the option of duodenal switch weight loss surgery. Schedule a consult today to find out more.
Who Is a Good Candidate for Duodenal Switch Surgery?
The surgery is complex and tends to result in a long recovery time – about three to four weeks – but patients can lose between 60 to 80 percent of their excess weight throughout a period of one year to 18 months after the procedure, according to the National Bariatric Link.*
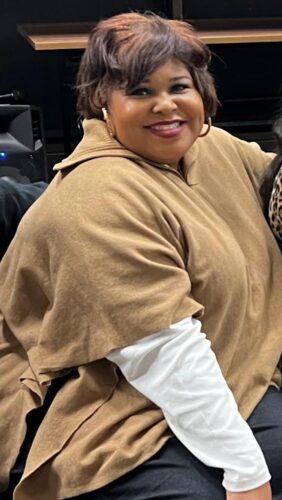
Patient Results
Qualifications for the Duodenal Switch Procedure
Suitable candidates should have a body mass index (BMI) of more than 40, according to the National Bariatric Link. The surgery tends to be most effective and, therefore, the preferred procedure for people with particularly high BMIs, of higher than 50, or with other metabolic health conditions, such as diabetes. If a candidate has a BMI lower than 40 but wishes to resolve other weight-related medical problems, DS is an option.
The best candidates for DS are between the ages of 18 and 65. However, choosing the appropriate weight-loss method – especially something drastic like a bariatric surgery – comes down to more than one’s BMI.
Those weighing their options for bariatric surgery should take a few other things into consideration before deciding to pursue a DS procedure. For instance, individuals suffering from gastroesophageal reflux disease (GERD) or inflammatory bowel disease (IBD) should speak with a surgeon first, as those conditions may pose a threat.
Additionally, DS patients will rely on dietary and nutrition supplements for the rest of their lives, so they must be sticklers about taking medications exactly as prescribed and following their Dr. Bagshahi’s post-surgery guidelines. Not doing so could have severe implications to their health because daily bariatric vitamins, as well as other medications, are necessary to avoid malnutrition and long-term vitamin and mineral deficiencies, according to the Bariatric Surgery Source.
Vegans and vegetarians also should be careful when choosing DS surgery, as they may be particularly at-risk for protein deficiency unless they make sure to get adequate protein from non-meat sources.
Patient Reviews
[rmrrsc type=”single” reviews=”4858794094326406933.GOOGLEMYBUSINESS-1062853175″]
Duodenal Switch vs. Gastric Sleeve Weight Loss Surgeries
It’s important to note that duodenal switch surgery is often performed in complement with gastric sleeve techniques to obtain the best quality of results. The right approach varies from patient to patient and Dr. Bagshahi will speak with you at length about the most optimal treatment plan to achieve an ideal outcome according to your needs. That said, if you are considering bariatric weight loss surgery, exploring the differences between the duodenal switch vs. gastric sleeve procedures will help you become informed regarding your options. The first aspect of the duodenal switch procedure is very similar to the gastric sleeve surgery.
While both are known to produce long term weight losses in severely obese individuals, the duodenal switch surgery produces the largest amount of long term weight loss and is best at treating obesity-related conditions such as diabetes.
Short and long term complications are higher for the duodenal switch when compared to the gastric sleeve procedure, therefore, the latter is often the bariatric surgery of choice for obese people who are not also dealing with a severe illness such as diabetes.
The Gastric Sleeve Procedure Explained
During a gastric sleeve surgery, also known as the laparoscopic sleeve gastrectomy, your surgeon will remove approximately 80% of your stomach and leave behind a tubular pouch that is shaped like a sleeve. The remaining stomach material is stapled together to form your new stomach which will fully heal over time. Unlike the gastric bypass procedure, your pyloric valve (the valve between your stomach and small intestine) is left intact.
Similar to the other surgeries described above, the BPD/DS initially helps to reduce the amount of food that is consumed; however, over time this effect lessens and patients are able to eventually consume near “normal” amounts of food. Unlike the other procedures, there is a significant amount of small bowel that is bypassed by the food stream.
Additionally, the food does not mix with the bile and pancreatic enzymes until very far down the small intestine. This results in a significant decrease in the absorption of calories and nutrients (particularly protein and fat) as well as nutrients and vitamins dependent on fat for absorption (fat soluble vitamins and nutrients).
Lastly, the BPD/DS, similar to the gastric bypass and sleeve gastrectomy, affects guts hormones in a manner that impacts hunger and satiety as well as blood sugar control. The BPD/DS is considered to be the most effective surgery for the treatment of diabetes among those that are described here.
What Will My Diet After Duodenal Switch Surgery Be Like?
Following your surgery, your diet will likely consist of small meals that are high in protein content. You should avoid foods with added sugar or fat, instead opting for vegetables, eggs, lean proteins, fruits, whole grains, and low-fat meals. Since your body will be absorbing fewer nutrients as a result of the procedure, it’s critical that you also take your prescribed vitamin and mineral supplements on a daily basis. Dr. Bagshahi advises eating slowly and chewing thoroughly to improve digestion.
While you will only be able to consume smaller meals at first, your stomach should slowly stretch over time and allow you to eat larger portions. That said, it’s highly recommended to remain watchful of your caloric intake, avoid snacking, and stop eating as soon as you feel satisfied.
How Much Will Duodenal Switch Surgery Cost?
In the Fort Worth area, the cost of the duodenal switch procedure can range from $12,000 to $15,000, although the price of surgery is largely personalized according to each patient’s specific needs and weight loss goals. The estimation listed above includes the various expenses typically associated with bariatric surgery, such as fees for the anesthesia, post-operative care, hospital facility, surgeon, etc. Once Dr. Bagshahi confirms that duodenal switch surgery is the best treatment option for you, our office will be able to help you navigate the insurance process.
For all out-of-pocket expenses, our weight loss center also accepts financing plans from trusted bariatric surgery lenders like CareCredit®, United Medical Credit®, and Prosper® Healthcare Lending. If you qualify for financing, these companies can make your surgical costs more manageable by allowing you to choose from an array of flexible, low- to no-interest payment plans.
Our team is here to assist you with all of your questions and concerns regarding the cost of duodenal switch surgery, or our other weight loss treatment options. Please call (817) 631-2655 if you would like to speak to a member of our office, or to book a consultation.
What are Common Side Effects of the Duodenal Switch Procedure?
Duodenal switch surgery poses a risk of potential health complications just like any other major surgery. With the duodenal switch technique in particular, patients may face an increased risk of vitamin and mineral deficiencies. Other possible long-term complications may include:
- Malnutrition
- Bowel obstruction
- Dumping syndrome
- Ulcers
- Vomiting
- Hernias
- Gallstones
- Low blood sugar
Selecting a qualified and experienced bariatric surgeon to perform your procedure can help you avoid potential complications before and after surgery. Dr. Bagshahi will review your medical history to help you determine the most ideal bariatric treatment to safely and effectively achieve your weight loss goals.
What's the Difference Between Open vs. Laparoscopic Duodenal Switch Surgery?
The duodenal switch procedure can be performed as a traditional open surgery or with minimally invasive techniques, which is considered a laparoscopic approach. During open surgery, duodenal switch utilizes a long incision on the belly. This can lead to a longer recovery, more extensive scarring, and relatively more discomfort when compared to minimally invasive surgery.
When performed laparoscopically, your weight loss surgeon uses a narrow telescope with a lighted camera on the end (known as a “laparoscope”) to complete your procedure. Unlike open surgery, this only requires your surgeon to make tiny incisions in the treated areas, allowing a faster healing process, less discomfort, less extensive scarring, and a lower risk of complications when compared to a traditional duodenal switch procedure. The same benefits are also possible with robotic-assisted surgery using the daVinci® system, and the best approach for your needs can be determined in your consultation.
Are There Alternatives to Duodenal Switch Surgery?
Modern advances in bariatric surgery have given patients more options than ever before in meeting their weight loss goals. Determining which procedure is best for you is a process based on your starting weight, height, overall level of health, motivation level and more.
By discussing the pros and cons of each procedure with Dr. Bagshahi, you’ll be well on your way to selecting a procedure that can change your life for the better.
The Biliopancreatic Diversion with Duodenal Switch – abbreviated as BPD/DS – is a procedure with two components. First, a smaller, tubular stomach pouch is created by removing a portion of the stomach, very similar to the sleeve gastrectomy. Next, a large portion of the small intestine is bypassed.
Additional Duodenal Switch FAQs
How long will the results of duodenal switch surgery last?
The duodenal switch procedure permanently changes the digestive system and results are designed to yield long-term weight loss. On average, duodenal switch surgery has a 90 percent success rate for weight loss, meaning patients who undergo the procedure lose at least 50 percent of their body weight. Most individuals lose more than 50 percent. Better yet, the procedure also retains an up to 90 percent rate of remission for obesity-related conditions, such as Type 2 diabetes. Many patients are able to discontinue their intake of medications they were once reliant on, but outcomes vary from person to person.
What are good post-duodenal switch recipes?
Once you reach the final stage of the duodenal switch recovery and start reintroducing solid foods into your diet, it’s advised to consume low-fat and low-sugar meals. Recipes should be rich in proteins and vegetables. Patients should also avoid high-fat, greasy, or fried foods. You will receive extensive instructions regarding dietary restrictions after surgery. We also invite you to explore the healthy and delicious recipes found in our bariatric surgery blog.
What is the average recovery time after duodenal switch surgery?
Recovery after the duodenal switch procedure generally lasts a few weeks before patients feel well enough to return to work. Spending a few days in the hospital immediately after surgery is to be expected. During the recovery period, your body will undergo significant changes and weight loss may occur rapidly. Adjusting to stringent dietary guidelines will be a part of your recovery and inform the extent of weight loss experienced. Dr. Bagshahi will guide you through the recovery process through regular post-operative follow-up appointments.
Can the duodenal switch procedure be performed as a robotic surgery?
Yes, duodenal switch surgery can be performed with the assistance of the da Vinci® robot for patients who are good candidates for this technique. Robotic-assisted surgery is a laparoscopic approach that can result in shorter incisions, less scarring, and a faster and smoother recovery period than traditional open surgery. Dr. Bagshahi can discuss robotic-assisted surgery in further detail once he gains a sense of your needs and goals.
When will I start seeing weight loss after duodenal switch surgery?
The most weight loss usually occurs during the first three months after the duodenal switch procedure. While every patient varies, most individuals lose up to 30 percent of their excess body weight during this time. Weight loss generally shows down after three months and peaks between 12 and 18 months after surgery. The amount of excess weight shed may be as much as 75 to 85 percent when the final results are revealed.